January is National Cervical Health Awareness Month.
So, let’s talk cervix….
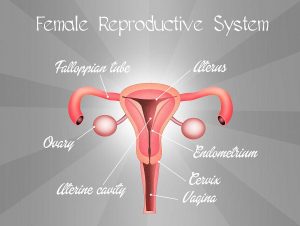
The cervix is part of the female reproductive system. It is a couple inches long and is connected to the uterus and vagina. It has a very small opening, the cervical os, that allows menstral flow to exit the body. Even more remarkable, it stretches wide enough to allow a full-sized baby to slide into the world. When a woman is in labor, the healthcare providers will assess the readiness of a women’s body to deliver by measuring the dilation of the cervix. The nurse or doctor will frequently perform internal exams to evaluate the diameter of the cervix os using a scale of 1 to 10 centimeters. When it is a “10”, it’s time to PUSH!
Unless your gynecologist whipped out a speculum and a mirror for your educational entertainment, you probably have not actually seen your cervix. Therefore, it is difficult for women to visualize and assess if something unhealthy is brewing. In addition, cervical cancer is often silent; there are no obvious signs and symptoms. This is why it is recommended to visit your healthcare provider on an annual basis.
According to the National Cervical Cancer Coalition, cancer of the cervix is diagnosed in about 12,000 U.S. women each year. Four thousand die. Globally, it is the second most common cancer among women. It is a highly preventable and treatable cancer when suggested health guidelines are followed.
Signs and Symptoms of Cervical Cancer
- Abnormal bleeding
- Abdominal pain
- Unusual discharge
- Painful sex
- Painful urination or increase in bathroom breaks
These symptoms indicate any one of a number of health issues, which is why a visit to your provider is necessary when you experience unusual manifestations.
Tests
The Pap smear is a swab sample of your cervix to detect any cancerous or pre-cancerous cells present. Since the introduction of Pap smears the 50’s, cancer rates in the U.S. have dropped about 60% among women of child-bearing age.
HPV screening involves a swab sample of your cervix as well, often at the same time as the Pap test. This screening is different, however, because it detects the DNA of human papillomavirus (HPV). HPV is the virus that causes cervical cancer. Recent research indicates that HPV testing be the primary screening for cervical cancer rather than the Pap smear. However, the combination of the two offers invaluable information to your provider.
A woman may have a negative pap and positive HPV test, Positive pap and negative HPV, or both negative or both positive.
Treatment
Depending on the result, your healthcare provider will suggest treatment; often a wait-and-see approach is taken. This type of pre-cancerous cell grows slowly, so waiting a few months or a year to see if the test results are different is pretty standard. However, your provider might suggest removing the questionable cells with a follow-up procedure shortly thereafter. It all depends on the test results and what your provider observes during exam.

Prevention
Regular visits to your healthcare provider for screening is invaluable. Identifying and removing rogue cells early will save your life.
Screening Guidelines:
-Beginning at age 21, women should have a Pap smear every three years until approximately age 65. For older women, even if sex is not a part of their current lifestyle, continue to be tested as cervical cancer it may present itself two decades after exposure to HPV.
-Up to age 30, a Pap smear every 3 years is all that is necessary, depending on personal medical history and doctor’s recommendation.
-After age 30, an HPV screening test and Pap smear may be used together to screen women for cervical cancer. If both tests are negative, the next screening is typically at five years.
-Alternatively, if only an HPV screening is done, it should be repeated every three years, much like the Pap smear.
-Confused? Don’t be. Talk to you healthcare provider to come up with a plan that works with your comfort level and medical history. The days of annual Pap smears are over, however, so do not fret when providers suggest waiting a few years in between tests, but not exams.
Dr. Carolyn Mills, an Obstetrician and Gynecologist at Dreyer Medical Clinic in the Chicago suburbs, recommends women not neglect their annual gynecological exam between HPV and Pap screenings.
An annual exam is an excellent opportunity to talk with your healthcare provider about ongoing issues regarding contraception, breast health, and reproductive health. Additionally, there are other reproductive health issues that may be caught early by the health professional. For example, STI’s in general do not always present with symptoms; taking the time to give your healthcare provider an honest sexual history is imperative to receiving the excellent care every woman deserves.
On a personal note, I have always scheduled my exams during the month of May, the month I celebrate my birthday. Why? It is easy to remember, but honestly, what better gift can a person give themselves than the gift of good health? Well, shoes. There’s that, too. Take a “Me Day” and visit your gynecologist, your favorite shoe store, and perhaps lunch with a friend during your birthday month. In one glorious day a woman can address her physical, mental/emotional, and social wellness needs.
Vaccinations:
The HPV vaccine was introduced within the last decade. This vaccine prevents the specific strains of HPV that cause cancer (cervical, anal, penis, oral) and genital warts from taking hold. This vaccine is given in a series of three doses over six months to both males and females. However, even with the coverage the vaccine offers, it is not 100% effective. It is necessary to continue with your Pap smears and/or HPV tests.
At the age of 11 or 12, young people are able to receive a vaccine to prevent certain strains of HPV from causing genitals warts and a variety of cancers, including cervical cancer. This immunization is a series of three injections over the course of six months. The key is to vaccinate children before they become sexually active and are exposed to HPV. This vaccine is approved to be given up to the age of 26; if a person only received one or two injections of the series of three, they are able to finish out the regimen as a young adult. The vaccines are Gardasil, Gardasil 9, and Cervarix.
Cervical cancer used to be a leading cause of death among women in their child-bearing age. With the introduction of the Pap smear in the 1950’s, that number decreased about 60% according to the National Institute of Health. However, despite health care professional’s best efforts, it is the number two cancer among women worldwide. In the U.S., with the introduction of HPV screenings and the HPV vaccine, those numbers are expected to decline rapidly. Continue to visit your healthcare provider on a regular basis and discuss with them your plan of action to help prevent this treatable and preventable cancer.
For a candid and honest reflection of a woman who has undergone treatment for cervical cancer, read the upcoming interview “A Moment with Marcy: A Cervical Cancer Survivor’s Thoughtful Reflection”.
For more information about HPV read my article, “HPV Vaccine: Know the facts, make the choice” soon to be published in Kids In The House.